Effects of Post-Exertional Malaise on Markers of Arterial Stiffness in Individuals with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
International Journal of environmental research and public health.
Joshua Bond, Tessa Nielsen, and Lynette Hodges
Abstract
Background: Evidence is emerging that individuals with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) may suffer from chronic vascular dysfunction as a result of illness-related oxidative stress and vascular inflammation. The study aimed to examine the impact of maximal-intensity aerobic exercise on vascular function 48 and 72 h into recovery. Methods:ME/CFS (n = 11) with gender and age-matched controls (n = 11) were randomly assigned to either a 48 h or 72 h protocol. Each participant had measures of brachial blood pressure, augmentation index (AIx75, standardized to 75 bpm) and carotid-radial pulse wave velocity (crPWV) taken. This was followed by a maximal incremental cycle exercise test. Resting measures were repeated 48 or 72 h later (depending on group allocation). Results: No significant differences were found when ME/CFS were directly compared to controls at baseline. During recovery, the 48 h control group experienced a significant 7.2% reduction in AIx75 from baseline measures (p < 0.05), while the matched ME/CFS experienced no change in AIx75. The 72 h ME/CFS group experienced a non-significant increase of 1.4% from baseline measures. The 48 h and 72 h ME/CFS groups both experienced non-significant improvements in crPWV (0.56 ms−1 and 1.55 ms−1, respectively). Conclusions: The findings suggest that those with ME/CFS may not experience exercise-induced vasodilation due to chronic vascular damage, which may be a contributor to the onset of post-exertional malaise (PEM).
Keywords: myalgic encephalomyelitis, chronic fatigue syndrome, arterial stiffness, post-exertional malaise
________________________________________________________________________________
Mortality of people with chronic fatigue syndrome: a retrospective cohort study in England and Wales from the South London and Maudsley NHS Foundation Trust Biomedical Research Centre (SLaM BRC) Clinical Record Interactive Search (CRIS) Register
Emmert Roberts, Simon Wessely, Trudie Chalder, Chin-Kuo Chang*, Matthew Hotopf*
Lancet 2016; 387: 1638–43
Summary
Background
Mortality associated with chronic fatigue syndrome is uncertain. We investigated mortality in individuals diagnosed with chronic fatigue syndrome in secondary and tertiary care using data from the South London and Maudsley NHS Foundation Trust Biomedical Research Centre (SLaM BRC) Clinical Record Interactive Search (CRIS) register.
Methods We calculated standardised mortality ratios (SMRs) for all-cause, suicide-specific, and cancer-specific mortality for a 7-year observation period using the number of deaths observed in SLaM records compared with age specific and sex-specific mortality statistics for England and Wales. Study participants were included if they had had contact with the chronic fatigue service (referral, discharge, or case note entry) and received a diagnosis of chronic fatigue syndrome.
Findings
We identified 2147 cases of chronic fatigue syndrome from CRIS and 17 deaths from Jan 1, 2007, to Dec 31, 2013. 1533 patients were women of whom 11 died, and 614 were men of whom six died. There was no significant difference in age-standardised and sex-standardised mortality ratios (SMRs) for all-cause mortality (SMR 1·14, 95% CI 0·65–1·85; p=0·67) or cancer-specific mortality (1·39, 0·60–2·73; p=0·45) in patients with chronic fatigue syndrome when compared with the general population in England and Wales. This remained the case when deaths from suicide were removed from the analysis. There was a significant increase in suicide-specific mortality (SMR 6·85, 95% CI 2·22–15·98; p=0·002).
Interpretation
We did not note increased all-cause mortality in people with chronic fatigue syndrome, but our findings show a substantial increase in mortality from suicide. This highlights the need for clinicians to be aware of the increased risk of completed suicide and to assess suicidality adequately in patients with chronic fatigue syndrome.
________________________________________________________________________________
2021 Mar 22;8:642710.Front. Med. Lausanne.
doi: 10.3389/fmed.2021.642710. eCollection 2021.
Reduced Endothelial Function in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome-Results From Open-Label Cyclophosphamide Intervention Study
Kari Sørland 1 2, Miriam Kristine Sandvik 3, Ingrid Gurvin Rekeland 1 4, Lis Ribu 2, Milada Cvancarova Småstuen 2, Olav Mella 1 4, Øystein Fluge 1 4
PMID: 33829023 PMCID: PMC8019750 DOI: 10.3389/fmed.2021.642710
Abstract
Introduction: Patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) present with a range of symptoms including post-exertional malaise (PEM), orthostatic intolerance, and autonomic dysfunction. Dysfunction of the blood vessel endothelium could be an underlying biological mechanism, resulting in inability to fine-tune regulation of blood flow according to the metabolic demands of tissues. The objectives of the present study were to investigate endothelial function in ME/CFS patients compared to healthy individuals, and assess possible changes in endothelial function after intervention with IV cyclophosphamide. Methods: This substudy to the open-label phase II trial "Cyclophosphamide in ME/CFS" included 40 patients with mild-moderate to severe ME/CFS according to Canadian consensus criteria, aged 18-65 years. Endothelial function was measured by Flow-mediated dilation (FMD) and Post-occlusive reactive hyperemia (PORH) at baseline and repeated after 12 months. Endothelial function at baseline was compared with two cohorts of healthy controls (N = 66 and N = 30) from previous studies. Changes in endothelial function after 12 months were assessed and correlated with clinical response to cyclophosphamide. Biological markers for endothelial function were measured in serum at baseline and compared with healthy controls (N = 30). Results: Baseline FMD was significantly reduced in patients (median FMD 5.9%, range 0.5-13.1, n = 35) compared to healthy individuals (median FMD 7.7%, range 0.7-21, n = 66) (p = 0.005), as was PORH with patient score median 1,331 p.u. (range 343-4,334) vs. healthy individuals 1,886 p.u. (range 808-8,158) (p = 0.003). No significant associations were found between clinical response to cyclophosphamide intervention (reported in 55% of patients) and changes in FMD/PORH from baseline to 12 months. Serum levels of metabolites associated with endothelial dysfunction showed no significant differences between ME/CFS patients and healthy controls.
Conclusions: Patients with ME/CFS had reduced endothelial function affecting both large and small vessels compared to healthy controls. Changes in endothelial function did not follow clinical responses during follow-up after cyclophosphamide IV intervention.
________________________________________________________________________________
Intramuscular Pressure Is Almost Three Times Higher in Fibromyalgia Patients: A Possible Mechanism for Understanding the Muscle Pain and Tenderness
Robert S. Katz, Frank Leavitt, Alexandra Katz Small and Ben J. Small
The Journal of Rheumatology April 2021, 48 (4) 598-602; DOI: https://doi.org/10.3899/jrheum.191068
Abstract
Objective Widespread pain in fibromyalgia syndrome (FMS) is conventionally viewed as arising from disordered central processing. This study examines intramuscular pressure in the trapezius as an alternative mechanism for understanding FMS pain.
Methods One hundred eight patients who satisfied the American College of Rheumatology criteria for FMS and 30 patients who met the ACR criteria for another rheumatic disease comprised the study groups. Muscle pressure was measured in mmHg using a pressure gauge attached to a no. 22 needle inserted into the mid-portion of the trapezius muscle. In addition, patients with FMS and rheumatic disease controls had dolorimetry testing, digital palpation, and reported pain scores.
Results Muscle pressure was substantially higher in patients with FMS with a mean value of 33.48 ± 5.90 mmHg. Only 2 of 108 patients had muscle pressure of < 23 mmHg. The mean pressure in rheumatic disease controls was 12.23 ± 3.75 mmHg, with a range from 3–22 mmHg. Patients with FMS were more tender than controls based on both dolorimetry (P < 0.001) and digital palpation (P < 0.001). The mean pain score in patients with FMS and controls was 6.68 ± 1.91 and 1.43 ± 1.79, respectively (P < 0.001).
Conclusion Pressure in the trapezius muscle of patients with FMS is remarkably elevated and may be an intrinsic feature of FMS that could be monitored as part of the diagnostic evaluation. The burden of the pressure abnormality may help explain the diffuse muscle pain of FMS. Therefore, FMS as a disorder of exclusively central pain processing should be revisited. Therapeutically, the reduction of muscle pressure may change the clinical picture significantly.
________________________________________________________________________________
021 Apr 12;archdischild-2020-320196.
Recovery from chronic fatigue syndrome: a systematic review-heterogeneity of definition limits study comparison
Yasmin Moore 1, Teona Serafimova 1, Nina Anderson 1 2, Hayley King 1, Alison Richards 1 3, Amberly Brigden 1, Parisa Sinai 1, Julian Higgins 1, Caitlin Ascough 1, Philippa Clery 1, Esther M Crawley 4 5
PMID: 33846138 DOI: 10.1136/archdischild-2020-320196
Abstract
Background: Paediatric chronic fatigue syndrome or myalgic encephalomyelitis (CFS/ME) is a common illness with a major impact on quality of life. Recovery is poorly understood. Our aim was to describe definitions of recovery in paediatric CFS/ME, the rate of recovery and the time to recovery.
Methods: This systematic review included a detailed search of MEDLINE, EMBASE, PsycInfo and Cochrane Library between 1994 and July 2018. Inclusion criteria were (1) clinical trials and observational studies, (2) participants aged <19 years with CFS/ME, (3) conducted in Western Healthcare systems and (4) studies including a measure of recovery and time taken to recover.
Results: Twelve papers (10 studies) were identified, involving 826 patients (range 23-135). Recovery rates were highly varied, ranging between 4.5% and 83%.Eleven distinct definitions of recovery were used; six were composite outcomes while five used unidimensional outcomes. Outcome measures used to define recovery were highly heterogeneous. School attendance (n=8), fatigue (n=6) and physical functioning (n=4) were the most common outcomes included in definition of recovery. Only five definitions included a personal measure of recovery.
Implications: Definitions of recovery are highly variable, likely secondary to differences in study design, outcomes used, follow-up and study populations. Heterogeneous definitions of recovery limit meaningful comparison between studies, highlighting the need for a consensus definition going forward. Recovery is probably best defined from the child's own perspective with a single self-reported measure. If composite measures are used for research, there should be agreement on the core outcome set used.
________________________________________________________________________________
Journal of the Neurological Sciences Volume 422, 15 March 2021, 117326
Modulatory effects of cognitive exertion on regional functional connectivity of the salience network in women with ME/CFS: A pilot study
RiccardoMancaa1KatijaKhanb1MicaelaMitolocMatteo De MarcoaLynseyGrievesondRosemaryVarleyeIain D.WilkinsonfAnnalenaVenneria
https://doi.org/10.1016/j.jns.2021.117326
Highlights
Cognitive effort can induce PEM and worsening of ME/CFS symptoms.
PEM is associated with changes in functional connectivity of the salience network.
Increased right insular FC with frontal areas is associated with symptom worsening.
Abstract
Background
A common symptom of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is post-exertional malaise (PEM). Various brain abnormalities have been observed in patients with ME/CFS, especially in insular and limbic areas, but their link with ME/CFS symptoms is still unclear. This pilot study aimed at investigating the association between PEM in ME/CFS and changes in functional connectivity (FC) of two main networks: the salience network (SN) and the default-mode network (DMN).
Methods
A total of 16 women, 6 with and 10 without ME/CFS, underwent clinical and MRI assessment before and after cognitive exertion. Resting-state FC maps of 7 seeds (3 for the SN and 4 for the DMN) and clinical measures of fatigue, pain and cognition were analysed with repeated-measure models. FC-symptom change associations were also investigated.
Results
Exertion induced increases in fatigue and pain in patients with ME/CFS compared to the control group, while no changes were found in cognitive performance. At baseline, patients showed altered FC between some DMN seeds and frontal areas and stronger FC between all SN seeds and left temporal areas and the medulla. Significantly higher FC increases in patients than in controls were found only between the right insular seed and frontal and subcortical areas; these increases correlated with worsening of symptoms.
Conclusions
Cognitive exertion can induce worsening of ME/CFS-related symptoms. These changes were here associated with strengthening of FC of the right insula with areas involved in reward processing and cognitive control.
________________________________________________________________________________
Dysregulated Provision of Oxidisable Substrates to the Mitochondria in ME/CFS Lymphoblasts
Daniel Missailidis,Oana Sanislav,Claire Y. Allan,Paige K. Smith,Sarah J. Annesley,Paul R. Fisher
Department of Physiology, Anatomy and Microbiology, School of Life Sciences, La Trobe University, Melbourne, VIC 3086, Australia
Monash Health, Melbourne, VIC 3186, Australia
Int. J. Mol. Sci. 2021, 22(4), 2046; https://doi.org/10.3390/ijms22042046
Received: 16 January 2021 / Revised: 8 February 2021 / Accepted: 15 February 2021 / Published: 19 February 2021
Abstract
Although understanding of the biomedical basis of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is growing, the underlying pathological mechanisms remain uncertain. We recently reported a reduction in the proportion of basal oxygen consumption due to ATP synthesis by Complex V in ME/CFS patient-derived lymphoblast cell lines, suggesting mitochondrial respiratory inefficiency. This was accompanied by elevated respiratory capacity, elevated mammalian target of rapamycin complex 1 (mTORC1) signaling activity and elevated expression of enzymes involved in the TCA cycle, fatty acid β-oxidation and mitochondrial transport. These and other observations led us to hypothesise the dysregulation of pathways providing the mitochondria with oxidisable substrates. In our current study, we aimed to revisit this hypothesis by applying a combination of whole-cell transcriptomics, proteomics and energy stress signaling activity measures using subsets of up to 34 ME/CFS and 31 healthy control lymphoblast cell lines from our growing library. While levels of glycolytic enzymes were unchanged in accordance with our previous observations of unaltered glycolytic rates, the whole-cell proteomes of ME/CFS lymphoblasts contained elevated levels of enzymes involved in the TCA cycle (p = 1.03 × 10−4), the pentose phosphate pathway (p = 0.034, G6PD p = 5.5 × 10−4), mitochondrial fatty acid β-oxidation (p = 9.2 × 10−3), and degradation of amino acids including glutamine/glutamate (GLS p = 0.034, GLUD1 p = 0.048, GOT2 p = 0.026), branched-chain amino acids (BCKDHA p = 0.028, BCKDHB p = 0.031) and essential amino acids (FAH p = 0.036, GCDH p = 0.006). The activity of the major cellular energy stress sensor, AMPK, was elevated but the increase did not reach statistical significance. The results suggest that ME/CFS metabolism is dysregulated such that alternatives to glycolysis are more heavily utilised than in controls to provide the mitochondria with oxidisable substrates. View Full-Text
________________________________________________________________________________
Front Med (Lausanne) . 2021 Mar 22;8:642710. doi: 10.3389/fmed.2021.642710. eCollection 2021.
Reduced Endothelial Function in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome-Results From Open-Label Cyclophosphamide Intervention Study
Kari Sørland 1 2, Miriam Kristine Sandvik 3, Ingrid Gurvin Rekeland 1 4, Lis Ribu 2, Milada Cvancarova Småstuen 2, Olav Mella 1 4, Øystein Fluge 1 4
PMID: 33829023 PMCID: PMC8019750 DOI: 10.3389/fmed.2021.642710
Abstract
Introduction: Patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) present with a range of symptoms including post-exertional malaise (PEM), orthostatic intolerance, and autonomic dysfunction. Dysfunction of the blood vessel endothelium could be an underlying biological mechanism, resulting in inability to fine-tune regulation of blood flow according to the metabolic demands of tissues. The objectives of the present study were to investigate endothelial function in ME/CFS patients compared to healthy individuals, and assess possible changes in endothelial function after intervention with IV cyclophosphamide. Methods: This substudy to the open-label phase II trial "Cyclophosphamide in ME/CFS" included 40 patients with mild-moderate to severe ME/CFS according to Canadian consensus criteria, aged 18-65 years. Endothelial function was measured by Flow-mediated dilation (FMD) and Post-occlusive reactive hyperemia (PORH) at baseline and repeated after 12 months. Endothelial function at baseline was compared with two cohorts of healthy controls (N = 66 and N = 30) from previous studies. Changes in endothelial function after 12 months were assessed and correlated with clinical response to cyclophosphamide. Biological markers for endothelial function were measured in serum at baseline and compared with healthy controls (N = 30). Results: Baseline FMD was significantly reduced in patients (median FMD 5.9%, range 0.5-13.1, n = 35) compared to healthy individuals (median FMD 7.7%, range 0.7-21, n = 66) (p = 0.005), as was PORH with patient score median 1,331 p.u. (range 343-4,334) vs. healthy individuals 1,886 p.u. (range 808-8,158) (p = 0.003). No significant associations were found between clinical response to cyclophosphamide intervention (reported in 55% of patients) and changes in FMD/PORH from baseline to 12 months. Serum levels of metabolites associated with endothelial dysfunction showed no significant differences between ME/CFS patients and healthy controls. Conclusions: Patients with ME/CFS had reduced endothelial function affecting both large and small vessels compared to healthy controls. Changes in endothelial function did not follow clinical responses during follow-up after cyclophosphamide IV intervention.
________________________________________________________________________________
Aliment Pharmacol Ther 2021 Jan;53(1):79-86. doi: 10.1111/apt.16166. Epub 2020 Nov 18.
Randomised clinical trial: high-dose oral thiamine versus placebo for chronic fatigue in patients with quiescent inflammatory bowel disease
Palle Bager 1, Christian Lodberg Hvas 1, Charlotte Lock Rud 1, Jens Frederik Dahlerup 1
PMID: 33210299
Abstract
Background: Fatigue is a burdensome symptom for patients with inflammatory bowel disease (IBD). Few pharmacological interventions have documented effect on fatigue in patients with IBD. A pilot study indicated a 20-day effect with high-dose thiamine.
Aims: To investigate the effect and safety of high-dose oral thiamine (600-1800 mg/d) based on gender and weight on chronic fatigue in patients with quiescent IBD.
Methods: This was a randomised, double-blinded, placebo-controlled crossover trial. Patients had quiescent IBD, severe chronic fatigue and no other explanation for fatigue. Patients were allocated 1:1 to either 1) high-dose oral thiamine for 4 weeks, 4 weeks of washout, 4 weeks of oral placebo or 2) oral placebo for 4 weeks, 4 weeks of washout, 4 weeks of high-dose oral thiamine. Fatigue was measured using the Inflammatory Bowel Disease-Fatigue Questionnaire. The primary outcome was improvement (≥3 points) of fatigue after 4 weeks on thiamine.
Results: Forty patients were enrolled between November 2018 and October 2019. Crossover analysis showed a mean reduction of 4.5 points (95% CI 2.6-6.2) in fatigue after thiamine compared with a mean increase of 0.75 point (95% CI -1.3-2.8; P = 0.0003) after placebo. Furthermore, 55% of group 1 and 75% of group 2 showed an improvement ≥ 3 points while on thiamine compared with 25% of group 1 and 35% of group 2 while on placebo. Only mild side effects were detected.
Conclusion: We showed a significant beneficial effect of high-dose oral thiamine on chronic fatigue in IBD. The treatment was well tolerated.
________________________________________________________________________________
Mysterious Ailment, Mysterious Relief: Vaccines Help Some COVID Long Haulers
Will Stone – Kaiser Health News
April 16, 2021
.
An estimated 10% to 30% of people who get covid-19 suffer from lingering symptoms of the disease, or what's known as "long covid."
Judy Dodd, who lives in New York City, is one of them. She spent nearly a year plagued by headaches, shortness of breath, extreme fatigue and problems with her sense of smell, among other symptoms.
She said she worried that this "slog through life" was going to be her new normal.
Everything changed after she got her covid vaccine.
"I was like a new person. It was the craziest thing ever," said Dodd, referring to how many of her health problems subsided significantly after her second shot.
As the U.S. pushes to get people vaccinated, a curious benefit is emerging for those with this post-illness syndrome: Their symptoms are easing and, in some cases, fully resolving after vaccination.
It's the latest clue in the immunological puzzle of long covid, a still poorly understood condition that leaves some who get infected with wide-ranging symptoms months after the initial illness.
The notion that a vaccine aimed at preventing the disease may also treat it has sparked optimism among patients, and scientists who study the post-illness syndrome are taking a close look at these stories.
"I didn't expect the vaccine to make people feel better," said Akiko Iwasaki, an immunologist at the Yale School of Medicine who's researching long covid.
"More and more, I started hearing from people with long covid having their symptoms reduced or completely recovering, and that's when I started to get excited because this might be a potential cure for some people."
While promising, it's still too early to know just how many people with long covid feel better as a result of being vaccinated and whether that amounts to a statistically meaningful difference.
In the meantime, Iwasaki and other researchers are beginning to incorporate this question into ongoing studies of long haulers by monitoring their symptoms pre- and post-vaccination and collecting blood samples to study their immune response.
There are several leading theories for why vaccines could alleviate the symptoms of long covid: It's possible the vaccines clear up leftover virus or fragments, interrupt a damaging autoimmune response or in some other way "reset" the immune system.
"It's all biologically plausible and, importantly, should be easy to test," said Dr. Steven Deeks of the University of California-San Francisco, who is also studying the long-term impacts of the coronavirus on patients.
"
Among the patients of Dr. Daniel Griffin at Columbia University Medical Center in New York, "brain fog" and gastrointestinal problems are two of the most common symptoms that seem to resolve post-vaccination.
Griffin, who is running a long-term study of post-covid illness, initially estimated that about 30% to 40% of his patients felt better. Now, he believes the number may be higher, as more patients receive their second dose and see further improvements.
"We've been sort of chipping away at this [long covid] by treating each symptom," he said. "If it's really true that at least 40% of people have significant recovery with a therapeutic vaccination, then, to date, this is the most effective intervention we have for long covid."
A small U.K. study, not yet peer-reviewed, found about 23% of long-covid patients had an "increase in symptom resolution" post-vaccination, compared with about 15% of those who were unvaccinated.
But not all clinicians are seeing the same level of improvement.
Clinicians at post-covid clinics at the University of Washington in Seattle, Oregon Health & Science University in Portland, National Jewish Health in Denver and the University of Pittsburgh Medical Center told NPR and KHN that, so far, a small number of patients — or none at all — have reported feeling better after vaccination, but it wasn't a widespread phenomenon.
"I've heard anecdotes of people feeling worse, and you can scientifically come up with an explanation for it going in either direction," said UCSF's Deeks.
Why Are Patients Feeling Better?
There are several theories for why vaccines could help some patients — each relying on different physiological understandings of long covid, which manifests in a variety of ways.
"The clear story is that long covid isn't just one issue," said Dr. Eric Topol, director of the Scripps Research Translational Institute, which is also studying long covid and the possible therapeutic effects of vaccination.
Some people have fast resting heart rates and can't tolerate exercise. Others suffer primarily from cognitive problems, or some combination of symptoms like exhaustion, trouble sleeping and issues with smell and taste, he said.
As a result, it's likely that different therapies will work better for some versions of long covid than others, said Deeks.
One theory is that people who are infected never fully clear the coronavirus, and a viral "reservoir," or fragments of the virus, persist in parts of the body and cause inflammation and long-term symptoms, said Iwasaki, the Yale immunologist.
According to that explanation, the vaccine might induce an immune response that gives the body extra firepower to beat back the residual infection.
"That would actually be the most straightforward way of getting rid of the disease, because you're getting rid of the source of inflammation," Iwasaki said.
Griffin at Columbia Medical Center said this "viral persistence" idea is supported by what he's seeing in his patients and hearing from other researchers and clinicians. He said patients seem to be improving after receiving any of the covid vaccines, generally about "two weeks later, when it looks like they're having what would be an effective, protective response."
Another possible reason that some patients improve comes from the understanding of long covid as an autoimmune condition, in which the body's immune cells end up damaging its own tissues.
A vaccine could hypothetically kick into gear the "innate immune system" and "dampen the symptoms," but only temporarily, said Iwasaki, who has studied the role of harmful proteins, called autoantibodies, in covid.
This self-destructive immune response happens in a subset of covid patients while they are ill, and the autoantibodies produced can circulate for months later. But it's not yet clear how that may contribute to long covid, said John Wherry, director of the Institute for Immunology at the University of Pennsylvania.
Another theory is that the infection has "miswired" the immune system in some other way and caused chronic inflammation, perhaps like chronic fatigue syndrome, Wherry said. In that scenario, the vaccination might somehow "reset" the immune system.
________________________________________________________________________________
BMJ 2021; 372 doi: https://doi.org/10.1136/bmj.n693 (Published 31 March 2021)Cite this as: BMJ 2021;372:n693
Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study
Daniel Ayoubkhani, principal statistician1, Kamlesh Khunti, professor of primary care diabetes and vascular medicine2, Vahé Nafilyan, principal statistician1, Thomas Maddox, statistician1, Ben Humberstone, deputy director of health analysis and life events division1, Ian Diamond, UK national statistician1, Amitava Banerjee, associate professor of clinical data science and honorary consultant cardiologist
Accepted 15 March 2021
Abstract
Objective To quantify rates of organ specific dysfunction in individuals with covid-19 after discharge from hospital compared with a matched control group from the general population.
Design Retrospective cohort study.
Setting NHS hospitals in England.
Participants 47 780 individuals (mean age 65, 55% men) in hospital with covid-19 and discharged alive by 31 August 2020, exactly matched to controls from a pool of about 50 million people in England for personal and clinical characteristics from 10 years of electronic health records.
Main outcome measures Rates of hospital readmission (or any admission for controls), all cause mortality, and diagnoses of respiratory, cardiovascular, metabolic, kidney, and liver diseases until 30 September 2020. Variations in rate ratios by age, sex, and ethnicity.
Results Over a mean follow-up of 140 days, nearly a third of individuals who were discharged from hospital after acute covid-19 were readmitted (14 060 of 47 780) and more than 1 in 10 (5875) died after discharge, with these events occurring at rates four and eight times greater, respectively, than in the matched control group. Rates of respiratory disease (P<0.001), diabetes (P<0.001), and cardiovascular disease (P<0.001) were also significantly raised in patients with covid-19, with 770 (95% confidence interval 758 to 783), 127 (122 to 132), and 126 (121 to 131) diagnoses per 1000 person years, respectively. Rate ratios were greater for individuals aged less than 70 than for those aged 70 or older, and in ethnic minority groups compared with the white population, with the largest differences seen for respiratory disease (10.5 (95% confidence interval 9.7 to 11.4) for age less than 70 years v 4.6 (4.3 to 4.8) for age ≥70, and 11.4 (9.8 to 13.3) for non-white v 5.2 (5.0 to 5.5) for white individuals).
Conclusions Individuals discharged from hospital after covid-19 had increased rates of multiorgan dysfunction compared with the expected risk in the general population. The increase in risk was not confined to the elderly and was not uniform across ethnicities. The diagnosis, treatment, and prevention of post-covid syndrome requires integrated rather than organ or disease specific approaches, and urgent research is needed to establish the risk factors.
________________________________________________________________________________
Neural therapy for fibromyalgia: Myth or improving quality of life?
Elif Balevi Batur Tuğba Atan First published: 21 September 2020 https://doi.org/10.1111/ijcp.13719 International Journal of Clinical practice
Abstract
Background
Fibromyalgia is a common rheumatic disease, which is thought to be a neuroendocrine dysregulation disorder. Patients’ quality of life (QOL) is severely affected by this disease. Though neural therapy, as a treatment option, attempts to correct the underlying neuroendocrine dysfunction, yet there is no proven evidence of its effect on this disease. The present study aimed to evaluate the effectiveness of neural therapy on pain and functionality in patients with fibromyalgia.
Methods
The study was a 1‐year retrospective cohort study and held in physical medicine and rehabilitation clinics. A total of 60 female patients diagnosed with fibromyalgia were included. Sixty female patients with fibromyalgia were included in this study. Patients were divided into two groups; the first group (n = 30) received neural therapy, the second group (n = 30) received conventional physical therapy and each of the two groups received the same home exercise (stretching, strengthening and aerobic exercises) programme for four weeks. The primer outcomes were visual analogue scale (VAS), Short Form‐36 (SF‐36) and Fibromyalgia Impact Questionnaire (FIQ) scores after the treatment.
Results
The social functioning score exhibited a significant improvement only in the intra‐group comparison of the neural therapy group (P < .001). However, after treatment, the VAS, FIQ and all the SF‐36 parameters, except role limitations because of physical health, were detected to be significantly improved in the neural therapy group compared with the exercise group (P < .001).
Conclusions
Neural therapy may be an effective alternative treatment for improving the QOL in patients with fibromyalgia.
________________________________________________________________________________
Pharmacological Research
Volume 165, March 2021, 105465
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): Where will the drugs come from?
Peter L.ToogoodabDaniel J.ClauwcSameerPhadkebDavidHoffmand
https://doi.org/10.1016/j.phrs.2021.105465Get rights and content
Abstract
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a chronic debilitating disease characterized by severe and disabling fatigue that fails to improve with rest; it is commonly accompanied by multifocal pain, as well as sleep disruption, and cognitive dysfunction. Even mild exertion can exacerbate symptoms. The prevalence of ME/CFS in the U.S. is estimated to be 0.5–1.5 % and is higher among females. Viral infection is an established trigger for the onset of ME/CFS symptoms, raising the possibility of an increase in ME/CFS prevalence resulting from the ongoing COVID-19 pandemic. Current treatments are largely palliative and limited to alleviating symptoms and addressing the psychological sequelae associated with long-term disability. While ME/CFS is characterized by broad heterogeneity, common features include immune dysregulation and mitochondrial dysfunction. However, the underlying mechanistic basis of the disease remains poorly understood. Herein, we review the current understanding, diagnosis and treatment of ME/CFS and summarize past clinical studies aimed at identifying effective therapies. We describe the current status of mechanistic studies, including the identification of multiple targets for potential pharmacological intervention, and ongoing efforts towards the discovery of new medicines for ME/CFS treatment.
Graphical abstract
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): Where will the drugs come from? P. Toogood, D. Clauw, S. Phadke, D. Hoffman.
International Journal of environmental research and public health.
Joshua Bond, Tessa Nielsen, and Lynette Hodges
Abstract
Background: Evidence is emerging that individuals with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) may suffer from chronic vascular dysfunction as a result of illness-related oxidative stress and vascular inflammation. The study aimed to examine the impact of maximal-intensity aerobic exercise on vascular function 48 and 72 h into recovery. Methods:ME/CFS (n = 11) with gender and age-matched controls (n = 11) were randomly assigned to either a 48 h or 72 h protocol. Each participant had measures of brachial blood pressure, augmentation index (AIx75, standardized to 75 bpm) and carotid-radial pulse wave velocity (crPWV) taken. This was followed by a maximal incremental cycle exercise test. Resting measures were repeated 48 or 72 h later (depending on group allocation). Results: No significant differences were found when ME/CFS were directly compared to controls at baseline. During recovery, the 48 h control group experienced a significant 7.2% reduction in AIx75 from baseline measures (p < 0.05), while the matched ME/CFS experienced no change in AIx75. The 72 h ME/CFS group experienced a non-significant increase of 1.4% from baseline measures. The 48 h and 72 h ME/CFS groups both experienced non-significant improvements in crPWV (0.56 ms−1 and 1.55 ms−1, respectively). Conclusions: The findings suggest that those with ME/CFS may not experience exercise-induced vasodilation due to chronic vascular damage, which may be a contributor to the onset of post-exertional malaise (PEM).
Keywords: myalgic encephalomyelitis, chronic fatigue syndrome, arterial stiffness, post-exertional malaise
________________________________________________________________________________
Mortality of people with chronic fatigue syndrome: a retrospective cohort study in England and Wales from the South London and Maudsley NHS Foundation Trust Biomedical Research Centre (SLaM BRC) Clinical Record Interactive Search (CRIS) Register
Emmert Roberts, Simon Wessely, Trudie Chalder, Chin-Kuo Chang*, Matthew Hotopf*
Lancet 2016; 387: 1638–43
Summary
Background
Mortality associated with chronic fatigue syndrome is uncertain. We investigated mortality in individuals diagnosed with chronic fatigue syndrome in secondary and tertiary care using data from the South London and Maudsley NHS Foundation Trust Biomedical Research Centre (SLaM BRC) Clinical Record Interactive Search (CRIS) register.
Methods We calculated standardised mortality ratios (SMRs) for all-cause, suicide-specific, and cancer-specific mortality for a 7-year observation period using the number of deaths observed in SLaM records compared with age specific and sex-specific mortality statistics for England and Wales. Study participants were included if they had had contact with the chronic fatigue service (referral, discharge, or case note entry) and received a diagnosis of chronic fatigue syndrome.
Findings
We identified 2147 cases of chronic fatigue syndrome from CRIS and 17 deaths from Jan 1, 2007, to Dec 31, 2013. 1533 patients were women of whom 11 died, and 614 were men of whom six died. There was no significant difference in age-standardised and sex-standardised mortality ratios (SMRs) for all-cause mortality (SMR 1·14, 95% CI 0·65–1·85; p=0·67) or cancer-specific mortality (1·39, 0·60–2·73; p=0·45) in patients with chronic fatigue syndrome when compared with the general population in England and Wales. This remained the case when deaths from suicide were removed from the analysis. There was a significant increase in suicide-specific mortality (SMR 6·85, 95% CI 2·22–15·98; p=0·002).
Interpretation
We did not note increased all-cause mortality in people with chronic fatigue syndrome, but our findings show a substantial increase in mortality from suicide. This highlights the need for clinicians to be aware of the increased risk of completed suicide and to assess suicidality adequately in patients with chronic fatigue syndrome.
________________________________________________________________________________
2021 Mar 22;8:642710.Front. Med. Lausanne.
doi: 10.3389/fmed.2021.642710. eCollection 2021.
Reduced Endothelial Function in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome-Results From Open-Label Cyclophosphamide Intervention Study
Kari Sørland 1 2, Miriam Kristine Sandvik 3, Ingrid Gurvin Rekeland 1 4, Lis Ribu 2, Milada Cvancarova Småstuen 2, Olav Mella 1 4, Øystein Fluge 1 4
PMID: 33829023 PMCID: PMC8019750 DOI: 10.3389/fmed.2021.642710
Abstract
Introduction: Patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) present with a range of symptoms including post-exertional malaise (PEM), orthostatic intolerance, and autonomic dysfunction. Dysfunction of the blood vessel endothelium could be an underlying biological mechanism, resulting in inability to fine-tune regulation of blood flow according to the metabolic demands of tissues. The objectives of the present study were to investigate endothelial function in ME/CFS patients compared to healthy individuals, and assess possible changes in endothelial function after intervention with IV cyclophosphamide. Methods: This substudy to the open-label phase II trial "Cyclophosphamide in ME/CFS" included 40 patients with mild-moderate to severe ME/CFS according to Canadian consensus criteria, aged 18-65 years. Endothelial function was measured by Flow-mediated dilation (FMD) and Post-occlusive reactive hyperemia (PORH) at baseline and repeated after 12 months. Endothelial function at baseline was compared with two cohorts of healthy controls (N = 66 and N = 30) from previous studies. Changes in endothelial function after 12 months were assessed and correlated with clinical response to cyclophosphamide. Biological markers for endothelial function were measured in serum at baseline and compared with healthy controls (N = 30). Results: Baseline FMD was significantly reduced in patients (median FMD 5.9%, range 0.5-13.1, n = 35) compared to healthy individuals (median FMD 7.7%, range 0.7-21, n = 66) (p = 0.005), as was PORH with patient score median 1,331 p.u. (range 343-4,334) vs. healthy individuals 1,886 p.u. (range 808-8,158) (p = 0.003). No significant associations were found between clinical response to cyclophosphamide intervention (reported in 55% of patients) and changes in FMD/PORH from baseline to 12 months. Serum levels of metabolites associated with endothelial dysfunction showed no significant differences between ME/CFS patients and healthy controls.
Conclusions: Patients with ME/CFS had reduced endothelial function affecting both large and small vessels compared to healthy controls. Changes in endothelial function did not follow clinical responses during follow-up after cyclophosphamide IV intervention.
________________________________________________________________________________
Intramuscular Pressure Is Almost Three Times Higher in Fibromyalgia Patients: A Possible Mechanism for Understanding the Muscle Pain and Tenderness
Robert S. Katz, Frank Leavitt, Alexandra Katz Small and Ben J. Small
The Journal of Rheumatology April 2021, 48 (4) 598-602; DOI: https://doi.org/10.3899/jrheum.191068
Abstract
Objective Widespread pain in fibromyalgia syndrome (FMS) is conventionally viewed as arising from disordered central processing. This study examines intramuscular pressure in the trapezius as an alternative mechanism for understanding FMS pain.
Methods One hundred eight patients who satisfied the American College of Rheumatology criteria for FMS and 30 patients who met the ACR criteria for another rheumatic disease comprised the study groups. Muscle pressure was measured in mmHg using a pressure gauge attached to a no. 22 needle inserted into the mid-portion of the trapezius muscle. In addition, patients with FMS and rheumatic disease controls had dolorimetry testing, digital palpation, and reported pain scores.
Results Muscle pressure was substantially higher in patients with FMS with a mean value of 33.48 ± 5.90 mmHg. Only 2 of 108 patients had muscle pressure of < 23 mmHg. The mean pressure in rheumatic disease controls was 12.23 ± 3.75 mmHg, with a range from 3–22 mmHg. Patients with FMS were more tender than controls based on both dolorimetry (P < 0.001) and digital palpation (P < 0.001). The mean pain score in patients with FMS and controls was 6.68 ± 1.91 and 1.43 ± 1.79, respectively (P < 0.001).
Conclusion Pressure in the trapezius muscle of patients with FMS is remarkably elevated and may be an intrinsic feature of FMS that could be monitored as part of the diagnostic evaluation. The burden of the pressure abnormality may help explain the diffuse muscle pain of FMS. Therefore, FMS as a disorder of exclusively central pain processing should be revisited. Therapeutically, the reduction of muscle pressure may change the clinical picture significantly.
________________________________________________________________________________
021 Apr 12;archdischild-2020-320196.
Recovery from chronic fatigue syndrome: a systematic review-heterogeneity of definition limits study comparison
Yasmin Moore 1, Teona Serafimova 1, Nina Anderson 1 2, Hayley King 1, Alison Richards 1 3, Amberly Brigden 1, Parisa Sinai 1, Julian Higgins 1, Caitlin Ascough 1, Philippa Clery 1, Esther M Crawley 4 5
PMID: 33846138 DOI: 10.1136/archdischild-2020-320196
Abstract
Background: Paediatric chronic fatigue syndrome or myalgic encephalomyelitis (CFS/ME) is a common illness with a major impact on quality of life. Recovery is poorly understood. Our aim was to describe definitions of recovery in paediatric CFS/ME, the rate of recovery and the time to recovery.
Methods: This systematic review included a detailed search of MEDLINE, EMBASE, PsycInfo and Cochrane Library between 1994 and July 2018. Inclusion criteria were (1) clinical trials and observational studies, (2) participants aged <19 years with CFS/ME, (3) conducted in Western Healthcare systems and (4) studies including a measure of recovery and time taken to recover.
Results: Twelve papers (10 studies) were identified, involving 826 patients (range 23-135). Recovery rates were highly varied, ranging between 4.5% and 83%.Eleven distinct definitions of recovery were used; six were composite outcomes while five used unidimensional outcomes. Outcome measures used to define recovery were highly heterogeneous. School attendance (n=8), fatigue (n=6) and physical functioning (n=4) were the most common outcomes included in definition of recovery. Only five definitions included a personal measure of recovery.
Implications: Definitions of recovery are highly variable, likely secondary to differences in study design, outcomes used, follow-up and study populations. Heterogeneous definitions of recovery limit meaningful comparison between studies, highlighting the need for a consensus definition going forward. Recovery is probably best defined from the child's own perspective with a single self-reported measure. If composite measures are used for research, there should be agreement on the core outcome set used.
________________________________________________________________________________
Journal of the Neurological Sciences Volume 422, 15 March 2021, 117326
Modulatory effects of cognitive exertion on regional functional connectivity of the salience network in women with ME/CFS: A pilot study
RiccardoMancaa1KatijaKhanb1MicaelaMitolocMatteo De MarcoaLynseyGrievesondRosemaryVarleyeIain D.WilkinsonfAnnalenaVenneria
https://doi.org/10.1016/j.jns.2021.117326
Highlights
Cognitive effort can induce PEM and worsening of ME/CFS symptoms.
PEM is associated with changes in functional connectivity of the salience network.
Increased right insular FC with frontal areas is associated with symptom worsening.
Abstract
Background
A common symptom of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is post-exertional malaise (PEM). Various brain abnormalities have been observed in patients with ME/CFS, especially in insular and limbic areas, but their link with ME/CFS symptoms is still unclear. This pilot study aimed at investigating the association between PEM in ME/CFS and changes in functional connectivity (FC) of two main networks: the salience network (SN) and the default-mode network (DMN).
Methods
A total of 16 women, 6 with and 10 without ME/CFS, underwent clinical and MRI assessment before and after cognitive exertion. Resting-state FC maps of 7 seeds (3 for the SN and 4 for the DMN) and clinical measures of fatigue, pain and cognition were analysed with repeated-measure models. FC-symptom change associations were also investigated.
Results
Exertion induced increases in fatigue and pain in patients with ME/CFS compared to the control group, while no changes were found in cognitive performance. At baseline, patients showed altered FC between some DMN seeds and frontal areas and stronger FC between all SN seeds and left temporal areas and the medulla. Significantly higher FC increases in patients than in controls were found only between the right insular seed and frontal and subcortical areas; these increases correlated with worsening of symptoms.
Conclusions
Cognitive exertion can induce worsening of ME/CFS-related symptoms. These changes were here associated with strengthening of FC of the right insula with areas involved in reward processing and cognitive control.
________________________________________________________________________________
Dysregulated Provision of Oxidisable Substrates to the Mitochondria in ME/CFS Lymphoblasts
Daniel Missailidis,Oana Sanislav,Claire Y. Allan,Paige K. Smith,Sarah J. Annesley,Paul R. Fisher
Department of Physiology, Anatomy and Microbiology, School of Life Sciences, La Trobe University, Melbourne, VIC 3086, Australia
Monash Health, Melbourne, VIC 3186, Australia
Int. J. Mol. Sci. 2021, 22(4), 2046; https://doi.org/10.3390/ijms22042046
Received: 16 January 2021 / Revised: 8 February 2021 / Accepted: 15 February 2021 / Published: 19 February 2021
Abstract
Although understanding of the biomedical basis of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is growing, the underlying pathological mechanisms remain uncertain. We recently reported a reduction in the proportion of basal oxygen consumption due to ATP synthesis by Complex V in ME/CFS patient-derived lymphoblast cell lines, suggesting mitochondrial respiratory inefficiency. This was accompanied by elevated respiratory capacity, elevated mammalian target of rapamycin complex 1 (mTORC1) signaling activity and elevated expression of enzymes involved in the TCA cycle, fatty acid β-oxidation and mitochondrial transport. These and other observations led us to hypothesise the dysregulation of pathways providing the mitochondria with oxidisable substrates. In our current study, we aimed to revisit this hypothesis by applying a combination of whole-cell transcriptomics, proteomics and energy stress signaling activity measures using subsets of up to 34 ME/CFS and 31 healthy control lymphoblast cell lines from our growing library. While levels of glycolytic enzymes were unchanged in accordance with our previous observations of unaltered glycolytic rates, the whole-cell proteomes of ME/CFS lymphoblasts contained elevated levels of enzymes involved in the TCA cycle (p = 1.03 × 10−4), the pentose phosphate pathway (p = 0.034, G6PD p = 5.5 × 10−4), mitochondrial fatty acid β-oxidation (p = 9.2 × 10−3), and degradation of amino acids including glutamine/glutamate (GLS p = 0.034, GLUD1 p = 0.048, GOT2 p = 0.026), branched-chain amino acids (BCKDHA p = 0.028, BCKDHB p = 0.031) and essential amino acids (FAH p = 0.036, GCDH p = 0.006). The activity of the major cellular energy stress sensor, AMPK, was elevated but the increase did not reach statistical significance. The results suggest that ME/CFS metabolism is dysregulated such that alternatives to glycolysis are more heavily utilised than in controls to provide the mitochondria with oxidisable substrates. View Full-Text
________________________________________________________________________________
Front Med (Lausanne) . 2021 Mar 22;8:642710. doi: 10.3389/fmed.2021.642710. eCollection 2021.
Reduced Endothelial Function in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome-Results From Open-Label Cyclophosphamide Intervention Study
Kari Sørland 1 2, Miriam Kristine Sandvik 3, Ingrid Gurvin Rekeland 1 4, Lis Ribu 2, Milada Cvancarova Småstuen 2, Olav Mella 1 4, Øystein Fluge 1 4
PMID: 33829023 PMCID: PMC8019750 DOI: 10.3389/fmed.2021.642710
Abstract
Introduction: Patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) present with a range of symptoms including post-exertional malaise (PEM), orthostatic intolerance, and autonomic dysfunction. Dysfunction of the blood vessel endothelium could be an underlying biological mechanism, resulting in inability to fine-tune regulation of blood flow according to the metabolic demands of tissues. The objectives of the present study were to investigate endothelial function in ME/CFS patients compared to healthy individuals, and assess possible changes in endothelial function after intervention with IV cyclophosphamide. Methods: This substudy to the open-label phase II trial "Cyclophosphamide in ME/CFS" included 40 patients with mild-moderate to severe ME/CFS according to Canadian consensus criteria, aged 18-65 years. Endothelial function was measured by Flow-mediated dilation (FMD) and Post-occlusive reactive hyperemia (PORH) at baseline and repeated after 12 months. Endothelial function at baseline was compared with two cohorts of healthy controls (N = 66 and N = 30) from previous studies. Changes in endothelial function after 12 months were assessed and correlated with clinical response to cyclophosphamide. Biological markers for endothelial function were measured in serum at baseline and compared with healthy controls (N = 30). Results: Baseline FMD was significantly reduced in patients (median FMD 5.9%, range 0.5-13.1, n = 35) compared to healthy individuals (median FMD 7.7%, range 0.7-21, n = 66) (p = 0.005), as was PORH with patient score median 1,331 p.u. (range 343-4,334) vs. healthy individuals 1,886 p.u. (range 808-8,158) (p = 0.003). No significant associations were found between clinical response to cyclophosphamide intervention (reported in 55% of patients) and changes in FMD/PORH from baseline to 12 months. Serum levels of metabolites associated with endothelial dysfunction showed no significant differences between ME/CFS patients and healthy controls. Conclusions: Patients with ME/CFS had reduced endothelial function affecting both large and small vessels compared to healthy controls. Changes in endothelial function did not follow clinical responses during follow-up after cyclophosphamide IV intervention.
________________________________________________________________________________
Aliment Pharmacol Ther 2021 Jan;53(1):79-86. doi: 10.1111/apt.16166. Epub 2020 Nov 18.
Randomised clinical trial: high-dose oral thiamine versus placebo for chronic fatigue in patients with quiescent inflammatory bowel disease
Palle Bager 1, Christian Lodberg Hvas 1, Charlotte Lock Rud 1, Jens Frederik Dahlerup 1
PMID: 33210299
Abstract
Background: Fatigue is a burdensome symptom for patients with inflammatory bowel disease (IBD). Few pharmacological interventions have documented effect on fatigue in patients with IBD. A pilot study indicated a 20-day effect with high-dose thiamine.
Aims: To investigate the effect and safety of high-dose oral thiamine (600-1800 mg/d) based on gender and weight on chronic fatigue in patients with quiescent IBD.
Methods: This was a randomised, double-blinded, placebo-controlled crossover trial. Patients had quiescent IBD, severe chronic fatigue and no other explanation for fatigue. Patients were allocated 1:1 to either 1) high-dose oral thiamine for 4 weeks, 4 weeks of washout, 4 weeks of oral placebo or 2) oral placebo for 4 weeks, 4 weeks of washout, 4 weeks of high-dose oral thiamine. Fatigue was measured using the Inflammatory Bowel Disease-Fatigue Questionnaire. The primary outcome was improvement (≥3 points) of fatigue after 4 weeks on thiamine.
Results: Forty patients were enrolled between November 2018 and October 2019. Crossover analysis showed a mean reduction of 4.5 points (95% CI 2.6-6.2) in fatigue after thiamine compared with a mean increase of 0.75 point (95% CI -1.3-2.8; P = 0.0003) after placebo. Furthermore, 55% of group 1 and 75% of group 2 showed an improvement ≥ 3 points while on thiamine compared with 25% of group 1 and 35% of group 2 while on placebo. Only mild side effects were detected.
Conclusion: We showed a significant beneficial effect of high-dose oral thiamine on chronic fatigue in IBD. The treatment was well tolerated.
________________________________________________________________________________
Mysterious Ailment, Mysterious Relief: Vaccines Help Some COVID Long Haulers
Will Stone – Kaiser Health News
April 16, 2021
.
An estimated 10% to 30% of people who get covid-19 suffer from lingering symptoms of the disease, or what's known as "long covid."
Judy Dodd, who lives in New York City, is one of them. She spent nearly a year plagued by headaches, shortness of breath, extreme fatigue and problems with her sense of smell, among other symptoms.
She said she worried that this "slog through life" was going to be her new normal.
Everything changed after she got her covid vaccine.
"I was like a new person. It was the craziest thing ever," said Dodd, referring to how many of her health problems subsided significantly after her second shot.
As the U.S. pushes to get people vaccinated, a curious benefit is emerging for those with this post-illness syndrome: Their symptoms are easing and, in some cases, fully resolving after vaccination.
It's the latest clue in the immunological puzzle of long covid, a still poorly understood condition that leaves some who get infected with wide-ranging symptoms months after the initial illness.
The notion that a vaccine aimed at preventing the disease may also treat it has sparked optimism among patients, and scientists who study the post-illness syndrome are taking a close look at these stories.
"I didn't expect the vaccine to make people feel better," said Akiko Iwasaki, an immunologist at the Yale School of Medicine who's researching long covid.
"More and more, I started hearing from people with long covid having their symptoms reduced or completely recovering, and that's when I started to get excited because this might be a potential cure for some people."
While promising, it's still too early to know just how many people with long covid feel better as a result of being vaccinated and whether that amounts to a statistically meaningful difference.
In the meantime, Iwasaki and other researchers are beginning to incorporate this question into ongoing studies of long haulers by monitoring their symptoms pre- and post-vaccination and collecting blood samples to study their immune response.
There are several leading theories for why vaccines could alleviate the symptoms of long covid: It's possible the vaccines clear up leftover virus or fragments, interrupt a damaging autoimmune response or in some other way "reset" the immune system.
"It's all biologically plausible and, importantly, should be easy to test," said Dr. Steven Deeks of the University of California-San Francisco, who is also studying the long-term impacts of the coronavirus on patients.
"
Among the patients of Dr. Daniel Griffin at Columbia University Medical Center in New York, "brain fog" and gastrointestinal problems are two of the most common symptoms that seem to resolve post-vaccination.
Griffin, who is running a long-term study of post-covid illness, initially estimated that about 30% to 40% of his patients felt better. Now, he believes the number may be higher, as more patients receive their second dose and see further improvements.
"We've been sort of chipping away at this [long covid] by treating each symptom," he said. "If it's really true that at least 40% of people have significant recovery with a therapeutic vaccination, then, to date, this is the most effective intervention we have for long covid."
A small U.K. study, not yet peer-reviewed, found about 23% of long-covid patients had an "increase in symptom resolution" post-vaccination, compared with about 15% of those who were unvaccinated.
But not all clinicians are seeing the same level of improvement.
Clinicians at post-covid clinics at the University of Washington in Seattle, Oregon Health & Science University in Portland, National Jewish Health in Denver and the University of Pittsburgh Medical Center told NPR and KHN that, so far, a small number of patients — or none at all — have reported feeling better after vaccination, but it wasn't a widespread phenomenon.
"I've heard anecdotes of people feeling worse, and you can scientifically come up with an explanation for it going in either direction," said UCSF's Deeks.
Why Are Patients Feeling Better?
There are several theories for why vaccines could help some patients — each relying on different physiological understandings of long covid, which manifests in a variety of ways.
"The clear story is that long covid isn't just one issue," said Dr. Eric Topol, director of the Scripps Research Translational Institute, which is also studying long covid and the possible therapeutic effects of vaccination.
Some people have fast resting heart rates and can't tolerate exercise. Others suffer primarily from cognitive problems, or some combination of symptoms like exhaustion, trouble sleeping and issues with smell and taste, he said.
As a result, it's likely that different therapies will work better for some versions of long covid than others, said Deeks.
One theory is that people who are infected never fully clear the coronavirus, and a viral "reservoir," or fragments of the virus, persist in parts of the body and cause inflammation and long-term symptoms, said Iwasaki, the Yale immunologist.
According to that explanation, the vaccine might induce an immune response that gives the body extra firepower to beat back the residual infection.
"That would actually be the most straightforward way of getting rid of the disease, because you're getting rid of the source of inflammation," Iwasaki said.
Griffin at Columbia Medical Center said this "viral persistence" idea is supported by what he's seeing in his patients and hearing from other researchers and clinicians. He said patients seem to be improving after receiving any of the covid vaccines, generally about "two weeks later, when it looks like they're having what would be an effective, protective response."
Another possible reason that some patients improve comes from the understanding of long covid as an autoimmune condition, in which the body's immune cells end up damaging its own tissues.
A vaccine could hypothetically kick into gear the "innate immune system" and "dampen the symptoms," but only temporarily, said Iwasaki, who has studied the role of harmful proteins, called autoantibodies, in covid.
This self-destructive immune response happens in a subset of covid patients while they are ill, and the autoantibodies produced can circulate for months later. But it's not yet clear how that may contribute to long covid, said John Wherry, director of the Institute for Immunology at the University of Pennsylvania.
Another theory is that the infection has "miswired" the immune system in some other way and caused chronic inflammation, perhaps like chronic fatigue syndrome, Wherry said. In that scenario, the vaccination might somehow "reset" the immune system.
________________________________________________________________________________
BMJ 2021; 372 doi: https://doi.org/10.1136/bmj.n693 (Published 31 March 2021)Cite this as: BMJ 2021;372:n693
Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study
Daniel Ayoubkhani, principal statistician1, Kamlesh Khunti, professor of primary care diabetes and vascular medicine2, Vahé Nafilyan, principal statistician1, Thomas Maddox, statistician1, Ben Humberstone, deputy director of health analysis and life events division1, Ian Diamond, UK national statistician1, Amitava Banerjee, associate professor of clinical data science and honorary consultant cardiologist
Accepted 15 March 2021
Abstract
Objective To quantify rates of organ specific dysfunction in individuals with covid-19 after discharge from hospital compared with a matched control group from the general population.
Design Retrospective cohort study.
Setting NHS hospitals in England.
Participants 47 780 individuals (mean age 65, 55% men) in hospital with covid-19 and discharged alive by 31 August 2020, exactly matched to controls from a pool of about 50 million people in England for personal and clinical characteristics from 10 years of electronic health records.
Main outcome measures Rates of hospital readmission (or any admission for controls), all cause mortality, and diagnoses of respiratory, cardiovascular, metabolic, kidney, and liver diseases until 30 September 2020. Variations in rate ratios by age, sex, and ethnicity.
Results Over a mean follow-up of 140 days, nearly a third of individuals who were discharged from hospital after acute covid-19 were readmitted (14 060 of 47 780) and more than 1 in 10 (5875) died after discharge, with these events occurring at rates four and eight times greater, respectively, than in the matched control group. Rates of respiratory disease (P<0.001), diabetes (P<0.001), and cardiovascular disease (P<0.001) were also significantly raised in patients with covid-19, with 770 (95% confidence interval 758 to 783), 127 (122 to 132), and 126 (121 to 131) diagnoses per 1000 person years, respectively. Rate ratios were greater for individuals aged less than 70 than for those aged 70 or older, and in ethnic minority groups compared with the white population, with the largest differences seen for respiratory disease (10.5 (95% confidence interval 9.7 to 11.4) for age less than 70 years v 4.6 (4.3 to 4.8) for age ≥70, and 11.4 (9.8 to 13.3) for non-white v 5.2 (5.0 to 5.5) for white individuals).
Conclusions Individuals discharged from hospital after covid-19 had increased rates of multiorgan dysfunction compared with the expected risk in the general population. The increase in risk was not confined to the elderly and was not uniform across ethnicities. The diagnosis, treatment, and prevention of post-covid syndrome requires integrated rather than organ or disease specific approaches, and urgent research is needed to establish the risk factors.
________________________________________________________________________________
Neural therapy for fibromyalgia: Myth or improving quality of life?
Elif Balevi Batur Tuğba Atan First published: 21 September 2020 https://doi.org/10.1111/ijcp.13719 International Journal of Clinical practice
Abstract
Background
Fibromyalgia is a common rheumatic disease, which is thought to be a neuroendocrine dysregulation disorder. Patients’ quality of life (QOL) is severely affected by this disease. Though neural therapy, as a treatment option, attempts to correct the underlying neuroendocrine dysfunction, yet there is no proven evidence of its effect on this disease. The present study aimed to evaluate the effectiveness of neural therapy on pain and functionality in patients with fibromyalgia.
Methods
The study was a 1‐year retrospective cohort study and held in physical medicine and rehabilitation clinics. A total of 60 female patients diagnosed with fibromyalgia were included. Sixty female patients with fibromyalgia were included in this study. Patients were divided into two groups; the first group (n = 30) received neural therapy, the second group (n = 30) received conventional physical therapy and each of the two groups received the same home exercise (stretching, strengthening and aerobic exercises) programme for four weeks. The primer outcomes were visual analogue scale (VAS), Short Form‐36 (SF‐36) and Fibromyalgia Impact Questionnaire (FIQ) scores after the treatment.
Results
The social functioning score exhibited a significant improvement only in the intra‐group comparison of the neural therapy group (P < .001). However, after treatment, the VAS, FIQ and all the SF‐36 parameters, except role limitations because of physical health, were detected to be significantly improved in the neural therapy group compared with the exercise group (P < .001).
Conclusions
Neural therapy may be an effective alternative treatment for improving the QOL in patients with fibromyalgia.
________________________________________________________________________________
Pharmacological Research
Volume 165, March 2021, 105465
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): Where will the drugs come from?
Peter L.ToogoodabDaniel J.ClauwcSameerPhadkebDavidHoffmand
https://doi.org/10.1016/j.phrs.2021.105465Get rights and content
Abstract
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a chronic debilitating disease characterized by severe and disabling fatigue that fails to improve with rest; it is commonly accompanied by multifocal pain, as well as sleep disruption, and cognitive dysfunction. Even mild exertion can exacerbate symptoms. The prevalence of ME/CFS in the U.S. is estimated to be 0.5–1.5 % and is higher among females. Viral infection is an established trigger for the onset of ME/CFS symptoms, raising the possibility of an increase in ME/CFS prevalence resulting from the ongoing COVID-19 pandemic. Current treatments are largely palliative and limited to alleviating symptoms and addressing the psychological sequelae associated with long-term disability. While ME/CFS is characterized by broad heterogeneity, common features include immune dysregulation and mitochondrial dysfunction. However, the underlying mechanistic basis of the disease remains poorly understood. Herein, we review the current understanding, diagnosis and treatment of ME/CFS and summarize past clinical studies aimed at identifying effective therapies. We describe the current status of mechanistic studies, including the identification of multiple targets for potential pharmacological intervention, and ongoing efforts towards the discovery of new medicines for ME/CFS treatment.
Graphical abstract
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): Where will the drugs come from? P. Toogood, D. Clauw, S. Phadke, D. Hoffman.
________________________________________________________________________________
Antibody-dependent cell-mediated cytotoxicity (ADCC) in familial myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)
Alexander P. Sung,Jennifer J.-J. Tang,Michael J. Guglielmo,Julie Smith-Gagen,Lucinda Bateman ,Lydia Navarrete-Galvan, show all
Pages 226-244 | Received 17 Nov 2020, Accepted 12 Jan 2021, Published online: 02 Feb 2021
ABSTRACT
Background
Chronic fatigue syndrome (CFS) is an illness of unknown origin that may have familial risks. Low natural killer (NK) lymphocyte activity was proposed as a risk for familial CFS in 1998. Since then, there have been many studies of NK lymphocytes in CFS in general populations but few in familial CFS. Antibody-dependent cell-mediated cytotoxicity (ADCC) by NK lymphocytes helps control viral infections. ADCC is affected by variant CD16A receptors for antibody that are genetically encoded by FCGR3A.
Methods
This report characterizes ADCC effector NK cell numbers, ADCC activities, and FCGR3A variants of five families each with 2–5 CFS patients, their family members without CFS and unrelated controls. The patients met the Fukuda diagnostic criteria. We determined: CD16Apositive blood NK cell counts; EC50s for NK cell recognition of antibody; ADCC lytic capacity; FCGR3A alleles encoding CD16A variants, ROC tests for biomarkers, and synergistic risks.
Results
CFS patients and their family members had fewer CD16Apositive NK cells, required more antibody, and had ADCC that was lower than the unrelated controls. CFS family members were predominantly genetically CD16A F/F s for the variant with low affinity for antibodies. ROC tests indicated unsuitability of ADCC as a biomarker for CFS because of the low ADCC of family members without CFS. Familial synergistic risk vs. controls was evident for the combination of CD16Apositive NK cell counts with ADCC capacity.
Conclusions
Low ADCC may be a risk factor for familial CFS. Furthermore, characterization of familial CFS represents an opportunity to identify pathogenic mechanisms of CFS.
________________________________________________________________________________
Potential role of microbiome in Chronic Fatigue Syndrome/Myalgic Encephalomyelits (CFS/ME)
Giuseppe Francesco Damiano Lupo,Gabriele Rocchetti, Luigi Lucini, Lorenzo Lorusso, Elena Manara, Matteo Bertelli, Edoardo Puglisi & Enrica Capelli
Scientific Reports volume 11, Article number: 7043 (2021)
Abstract
Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME) is a severe multisystemic disease characterized by immunological abnormalities and dysfunction of energy metabolism. Recent evidences suggest strong correlations between dysbiosis and pathological condition. The present research explored the composition of the intestinal and oral microbiota in CFS/ME patients as compared to healthy controls. The fecal metabolomic profile of a subgroup of CFS/ME patients was also compared with the one of healthy controls. The fecal and salivary bacterial composition in CFS/ME patients was investigated by Illumina sequencing of 16S rRNA gene amplicons. The metabolomic analysis was performed by an UHPLC-MS. The fecal microbiota of CFS/ME patients showed a reduction of Lachnospiraceae, particularly Anaerostipes, and an increased abundance of genera Bacteroides and Phascolarctobacterium compared to the non-CFS/ME groups. The oral microbiota of CFS/ME patients showed an increase of Rothia dentocariosa. The fecal metabolomic profile of CFS/ME patients revealed high levels of glutamic acid and argininosuccinic acid, together with a decrease of alpha-tocopherol. Our results reveal microbial signatures of dysbiosis in the intestinal microbiota of CFS/ME patients. Further studies are needed to better understand if the microbial composition changes are cause or consequence of the onset of CFS/ME and if they are related to any of the several secondary symptoms.
________________________________________________________________________________
Perceptions of European ME/CFS Experts Concerning Knowledge and Understanding of ME/CFS among Primary Care Physicians in Europe: A Report from the European ME/CFS Research Network (EUROMENE)
John Cullinan 1, Derek F H Pheby 2, Diana Araja 3, Uldis Berkis 3, Elenka Brenna 4, Jean-Dominique de Korwin 5 6, Lara Gitto 7, Dyfrig A Hughes 8, Rachael M Hunter 9, Dominic Trepel 10 11, Xia Wang-Steverding 12 PMID: 33652747 PMCID: PMC7996783 DOI: 10.3390/medicina57030208
Abstract
Background and Objectives: We have conducted a survey of academic and clinical experts who are participants in the European ME/CFS Research Network (EUROMENE) to elicit perceptions of general practitioner (GP) knowledge and understanding of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and suggestions as to how this could be improved. Materials and Methods: A questionnaire was sent to all national representatives and members of the EUROMENE Core Group and Management Committee. Survey responses were collated and then summarized based on the numbers and percentages of respondents selecting each response option, while weighted average responses were calculated for questions with numerical value response options. Free text responses were analysed using thematic analysis. Results: Overall there were 23 responses to the survey from participants across 19 different European countries, with a 95% country-level response rate. Serious concerns were expressed about GPs' knowledge and understanding of ME/CFS, and, it was felt, about 60% of patients with ME/CFS went undiagnosed as a result. The vast majority of GPs were perceived to lack confidence in either diagnosing or managing the condition. Disbelief, and misleading illness attributions, were perceived to be widespread, and the unavailability of specialist centres to which GPs could refer patients and seek advice and support was frequently commented upon. There was widespread support for more training on ME/CFS at both undergraduate and postgraduate levels. Conclusion: The results of this survey are consistent with the existing scientific literature. ME/CFS experts report that lack of knowledge and understanding of ME/CFS among GPs is a major cause of missed and delayed diagnoses, which renders problematic attempts to determine the incidence and prevalence of the disease, and to measure its economic impact. It also contributes to the burden of disease through mismanagement in its early stages.
Keywords: GP knowledge and understanding; ME/CFS; chronic fatigue syndrome; myalgic encephalomyelitis; primary care.
________________________________________________________________________________
Clin Med. 2020 Oct 31;9(11):3527. doi: 10.3390/jcm9113527.
Evidence of Mitochondrial Dysfunction in Fibromyalgia: Deviating Muscle Energy Metabolism Detected Using Microdialysis and Magnetic Resonance
Björn Gerdle 1 2, Bijar Ghafouri 1, Eva Lund 3, Ann Bengtsson 1, Peter Lundberg 2 4, Helene van Ettinger-Veenstra 1 2, Olof Dahlqvist Leinhard 2 4 5, Mikael Fredrik Forsgren 2 4 5
Affiliations expand PMID: 33142767 PMCID: PMC7693920 DOI: 10.3390/jcm9113527
Abstract
In fibromyalgia (FM) muscle metabolism, studies are sparse and conflicting associations have been found between muscle metabolism and pain aspects. This study compared alterations in metabolic substances and blood flow in erector spinae and trapezius of FM patients and healthy controls. FM patients (n = 33) and healthy controls (n = 31) underwent a clinical examination that included pressure pain thresholds and physical tests, completion of a health questionnaire, participation in microdialysis investigations of the etrapezius and erector spinae muscles, and also underwent phosphorus-31 magnetic resonance spectroscopy of the erector spinae muscle. At the baseline, FM had significantly higher levels of pyruvate in both muscles. Significantly lower concentrations of phosphocreatine (PCr) and nucleotide triphosphate (mainly adenosine triphosphate) in erector spinae were found in FM. Blood flow in erector spinae was significantly lower in FM. Significant associations between metabolic variables and pain aspects (pain intensity and pressure pain threshold PPT) were found in FM. Our results suggest that FM has mitochondrial dysfunction, although it is unclear whether inactivity, obesity, aging, and pain are causes of, the results of, or coincidental to the mitochondrial dysfunction. The significant regressions of pain intensity and PPT in FM agree with other studies reporting associations between peripheral biological factors and pain aspects.
________________________________________________________________________________
Front. Med., 28 January 2021 | https://doi.org/10.3389/fmed.2021.628029
Hypothesis: Mechanisms That Prevent Recovery in Prolonged ICU Patients Also Underlie Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)
Dominic Stanculescu1, Lars Larsson2 and Jonas Bergquist3,4*
- 1Independent Researcher, Sint Martens Latem, Belgium
- 2Basic and Clinical Muscle Biology, Department of Physiology and Pharmacology, Karolinska Institute, Solna, Sweden
- 3Analytical Chemistry and Neurochemistry, Department of Chemistry – Biomedical Center, Uppsala University, Uppsala, Sweden
- 4The Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) Collaborative Research Centre at Uppsala University, Uppsala, Sweden
________________________________________________________________________________
Chest: 2021 Feb 10;S0012-3692(21)00256-7. doi: 10.1016/j.chest.2021.01.082.
Insights From Invasive Cardiopulmonary Exercise Testing of Patients With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
Phillip Joseph 1, Carlo Arevalo 2, Rudolf K F Oliveira 3, Mariana Faria-Urbina 4, Donna Felsenstein 5, Anne Louise Oaklander 6, David M Systrom 4 PMID: 33577778
Abstract
Background: Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) affects tens of millions worldwide; the causes of exertional intolerance are poorly understood. The ME/CFS label overlaps with postural orthostatic tachycardia (POTS) and fibromyalgia, and objective evidence of small fiber neuropathy (SFN) is reported in approximately 50% of POTS and fibromyalgia patients.
Research question: Can invasive cardiopulmonary exercise testing (iCPET) and PGP9.5-immunolabeled lower-leg skin biopsies inform the pathophysiology of ME/CFS exertional intolerance and potential relationships with SFN?
Study design and methods: We analyzed 1,516 upright invasive iCPETs performed to investigate exertional intolerance. After excluding patients with intrinsic heart or lung disease and selecting those with right atrial pressures (RAP) <6.5 mm Hg, results from 160 patients meeting ME/CFS criteria who had skin biopsy test results were compared with 36 control subjects. Rest-to-peak changes in cardiac output (Qc) were compared with oxygen uptake (Qc/VO2 slope) to identify participants with low, normal, or high pulmonary blood flow by Qc/VO2 tertiles.
Results: During exercise, the 160 ME/CFS patients averaged lower RAP (1.9 ± 2 vs 8.3 ± 1.5; P < .0001) and peak VO2 (80% ± 21% vs 101.4% ± 17%; P < .0001) than control subjects. The low-flow tertile had lower peak Qc than the normal and high-flow tertiles (88.4% ± 19% vs 99.5% ± 23.8% vs 99.9% ± 19.5% predicted; P < .01). In contrast, systemic oxygen extraction was impaired in high-flow vs low- and normal-flow participants (0.74% ± 0.1% vs 0.88 ± 0.11 vs 0.86 ± 0.1; P < .0001) in association with peripheral left-to-right shunting. Among the 160 ME/CFS patient biopsies, 31% were consistent with SFN (epidermal innervation ≤5.0% of predicted; P < .0001). Denervation severity did not correlate with exertional measures.
Interpretation: These results identify two types of peripheral neurovascular dysregulation that are biologically plausible contributors to ME/CFS exertional intolerance-depressed Qc from impaired venous return, and impaired peripheral oxygen extraction. In patients with small-fiber pathology, neuropathic dysregulation causing microvascular dilation may limit exertion by shunting oxygenated blood from capillary beds and reducing cardiac return.
________________________________________________________________________________
Healthcare (Basel) . 2020 Jun 30;8(3):192. doi: 10.3390/healthcare8030192.
Two-Day Cardiopulmonary Exercise Testing in Females with a Severe Grade of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Comparison with Patients with Mild and Moderate Disease
C Linda Mc van Campen 1, Peter C Rowe 2, Frans C Visser 1 PMID: 32629923 PMCID: PMC7551790
Abstract
Introduction: Effort intolerance along with a prolonged recovery from exercise and post-exertional exacerbation of symptoms are characteristic features of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). The gold standard to measure the degree of physical activity intolerance is cardiopulmonary exercise testing (CPET). Multiple studies have shown that peak oxygen consumption is reduced in the majority of ME/CFS patients, and that a 2-day CPET protocol further discriminates between ME/CFS patients and sedentary controls. Limited information is present on ME/CFS patients with a severe form of the disease. Therefore, the aim of this study was to compare the effects of a 2-day CPET protocol in female ME/CFS patients with a severe grade of the disease to mildly and moderately affected ME/CFS patients.
Methods and results: We studied 82 female patients who had undergone a 2-day CPET protocol. Measures of oxygen consumption (VO2), heart rate (HR) and workload both at peak exercise and at the ventilatory threshold (VT) were collected. ME/CFS disease severity was graded according to the International Consensus Criteria. Thirty-one patients were clinically graded as having mild disease, 31 with moderate and 20 with severe disease. Baseline characteristics did not differ between the 3 groups. Within each severity group, all analyzed CPET parameters (peak VO2, VO2 at VT, peak workload and the workload at VT) decreased significantly from day-1 to day-2 (p-Value between 0.003 and <0.0001). The magnitude of the change in CPET parameters from day-1 to day-2 was similar between mild, moderate, and severe groups, except for the difference in peak workload between mild and severe patients (p = 0.019). The peak workload decreases from day-1 to day-2 was largest in the severe ME/CFS group (-19 (11) %).
Conclusion: This relatively large 2-day CPET protocol study confirms previous findings of the reduction of various exercise variables in ME/CFS patients on day-2 testing. This is the first study to demonstrate that disease severity negatively influences exercise capacity in female ME/CFS patients. Finally, this study shows that the deterioration in peak workload from day-1 to day-2 is largest in the severe ME/CFS patient group.
________________________________________________________________________________
The impact of tryptophan supplementation on sleep quality: a systematic review, meta-analysis, and meta-regression
Clarinda N Sutanto, Wen Wei Loh, Jung Eun Kim
Nutrition Reviews, nuab027, https://doi.org/10.1093/nutrit/nuab027 Published: 03 May 2021
Abstract
Context
L-tryptophan (Trp) has been documented to aid sleep, but a systematic compilation of its effect on sleep quality is still limited.
Objective
We assessed the effect of Trp supplementation on sleep quality via meta-analysis and meta-regression. The effects of daily Trp dose (<1 g and ≥1 g) were also assessed.
Data sources
A database search was done in PubMed, Medline (Ovid), Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Cochrane and a total of 18 articles were collected.
Data extraction
Extracted data from 4 articles were also analyzed using random-effect meta-analysis and meta-regression. Standardized mean difference (SMD) was used in meta-analysis.
Data analysis
Results from the study suggested that Trp supplementation can shorten wake after sleep onset (−81.03 min/g, P = 0.017; SMD, −1.08 min [95%CI, −1.89 to −0.28]). In addition, the group receiving ≥1 g Trp supplementation had a shorter wake after sleep onset than the group with Trp < 1g supplementation (Trp <1 g vs Trp ≥1 g: 56.55 vs 28.91 min; P = 0.001). However, Trp supplementation did not affect other sleep components.
Conclusion
Trp supplementation, especially at ≥1 g can help improve sleep quality.
________________________________________________________________________________
COVID-19 symptoms over time: comparing long-haulers to ME/CFS
Leonard A. Jason,Mohammed F. Islam,Karl Conroy,Joseph Cotler,Chelsea Torres,Mady Johnson & show all
Received 21 Apr 2021, Accepted 22 Apr 2021, Published online: 05 May 2021
Fatigue,Biomedicine, Health and Behaviouir
ABSTRACT
Introduction
Our objective was to determine which symptoms among long-hauler COVID-19 patients change over time, and how their symptoms compare to another chronic illness group.
Methods
278 long-haulers completed two symptom questionnaires at one time point, with one recounting experiences during the first two weeks of their illness, an average of 21.7 weeks prior. We used a comparison group of 502 patients diagnosed with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Participants completed a standardized symptom questionnaire and a list of additional CDC COVID-19 symptoms.
Results
Over time, the long-haulers reported an overall reduction of most symptoms including unrefreshing sleep and post-exertional malaise, but an intensification of neurocognitive symptoms. When compared to ME/CFS, the COVID-19 sample was initially more symptomatic for the immune and orthostatic domains but over time, the long-haulers evidenced significantly less severe symptoms than those with ME/CFS, except in the orthostatic domain. Among the COVID-19 long haulers, several neurocognitive symptoms got worse over time, whereas improvements occurred in most other areas.
Conclusions
These types of differential patterns of symptoms over time might contribute to helping better understand the pathophysiology of those reporting prolonged illness following COVID-19.
________________________________________________________________________________
Sci Rep . 2021 Feb 25;11(1):4541. doi: 10.1038/s41598-021-83660-9.
Recursive ensemble feature selection provides a robust mRNA expression signature for myalgic encephalomyelitis/chronic fatigue syndrome
Paula I Metselaar 1, Lucero Mendoza-Maldonado 2, Andrew Yung Fong Li Yim 3, Ilias Abarkan 4, Peter Henneman 3, Anje A Te Velde 1, Alexander Schönhuth 5, Jos A Bosch 6 7, Aletta D Kraneveld 4, Alejandro Lopez-Rincon 8 9
Affiliations expand PMID: 33633136 PMCID: PMC7907358
Abstract
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a chronic disorder characterized by disabling fatigue. Several studies have sought to identify diagnostic biomarkers, with varying results. Here, we innovate this process by combining both mRNA expression and DNA methylation data. We performed recursive ensemble feature selection (REFS) on publicly available mRNA expression data in peripheral blood mononuclear cells (PBMCs) of 93 ME/CFS patients and 25 healthy controls, and found a signature of 23 genes capable of distinguishing cases and controls. REFS highly outperformed other methods, with an AUC of 0.92. We validated the results on a different platform (AUC of 0.95) and in DNA methylation data obtained from four public studies on ME/CFS (99 patients and 50 controls), identifying 48 gene-associated CpGs that predicted disease status as well (AUC of 0.97). Finally, ten of the 23 genes could be interpreted in the context of the derailed immune system of ME/CFS.
________________________________________________________________________________
Cytokine networks analysis uncovers further differences between those who develop myalgic encephalomyelitis/chronic fatigue syndrome following infectious mononucleosis
Leonard A. Jason,Joseph Cotler,Mohammed F. Islam,Jacob Furst,Matthew Sorenson &Ben Z. Katz
Pages 45-57 | Received 24 Feb 2021, Accepted 07 Apr 2021, Published online: 18 Apr 2021
https://doi.org/10.1080/21641846.2021.1915131
ABSTRACT
Background
We followed college students before, during, and after infectious mononucleosis (IM) for the development of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Aim
We used network analysis to study relationships between pre-illness cytokine data amongst three groups of participants: those 30 who went on to develop ME/CFS following IM (and met one case definition), those 18 who went on to develop severe ME/CFS (S-ME-CFS) following IM (and met greater than one case definition), and those 58 who recovered following IM (controls).
Methods
We recruited 4501 college students; approximately 5% developed IM during their enrollment at university. Those who developed IM were evaluated at a 6-month follow-up to determine whether they recovered or met criteria for ME/CFS; those who met >1 set of criteria for ME/CFS were termed S-ME/CFS. Patterns of pre-illness cytokine networks were then classified according to the following characteristics: membership, modularity, Eigen centrality, Total centrality, and mean degree. Network statistics were compared across groups using a one-way analysis of variance (ANOVA).
Results
Those with S-ME/CFS had a more interconnected network of cytokines, whereas recovered controls had more differentiated networks and more subgroupings of cytokine connections. Those with ME/CFS had a network that was denser than the controls, but less dense than those with severe ME/CFS.
Conclusions
The distinct network differences between these three groups implies that there may be biological differences between our three groups of study participants at baseline.
________________________________________________________________________________
Front. Med., 22 March 2021 | https://doi.org/10.3389/fmed.2021.642710
Reduced Endothelial Function in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome–Results From Open-Label Cyclophosphamide Intervention Study
Kari Sørland1,2*, Miriam Kristine Sandvik3, Ingrid Gurvin Rekeland1,4, Lis Ribu2, Milada Cvancarova Småstuen2, Olav Mella1,4 and Øystein Fluge1,4
- 1Department of Oncology and Medical Physics, Haukeland University Hospital, Bergen, Norway
- 2Faculty of Health Sciences, Oslo Metropolitan University, Oslo, Norway
- 3Porsgrunn District Psychiatric Centre, Telemark Hospital Trust, Porsgrunn, Norway
- 4Department of Clinical Science, Institute of Medicine, University of Bergen, Bergen, Norway
Methods: This substudy to the open-label phase II trial “Cyclophosphamide in ME/CFS” included 40 patients with mild-moderate to severe ME/CFS according to Canadian consensus criteria, aged 18–65 years. Endothelial function was measured by Flow-mediated dilation (FMD) and Post-occlusive reactive hyperemia (PORH) at baseline and repeated after 12 months. Endothelial function at baseline was compared with two cohorts of healthy controls (N = 66 and N = 30) from previous studies. Changes in endothelial function after 12 months were assessed and correlated with clinical response to cyclophosphamide. Biological markers for endothelial function were measured in serum at baseline and compared with healthy controls (N = 30).
Results: Baseline FMD was significantly reduced in patients (median FMD 5.9%, range 0.5–13.1, n = 35) compared to healthy individuals (median FMD 7.7%, range 0.7–21, n = 66) (p = 0.005), as was PORH with patient score median 1,331 p.u. (range 343–4,334) vs. healthy individuals 1,886 p.u. (range 808–8,158) (p = 0.003). No significant associations were found between clinical response to cyclophosphamide intervention (reported in 55% of patients) and changes in FMD/PORH from baseline to 12 months. Serum levels of metabolites associated with endothelial dysfunction showed no significant differences between ME/CFS patients and healthy controls.
Conclusions: Patients with ME/CFS had reduced endothelial function affecting both large and small vessels compared to healthy controls. Changes in endothelial function did not follow clinical responses during follow-up after cyclophosphamide IV intervention.
________________________________________________________________________________
Homebound versus Bedridden Status among Those with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
by Karl Conroy Shaun Bhatia Mohammed Islam and Leonard A. Jason
Center for Community Research, DePaul University, Chicago, IL 60614, USA
Healthcare 2021, 9(2), 106; https://doi.org/10.3390/healthcare9020106
Received: 29 December 2020 / Revised: 16 January 2021 / Accepted: 19 January 2021 / Published: 20 January 2021
(This article belongs to the Special Issue ME/CFS – the Severely and Very Severely Affected)
Abstract
Persons living with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) vary widely in terms of the severity of their illness. It is estimated that of those living with ME/CFS in the United States, about 385,000 are homebound. There is a need to know more about different degrees of being homebound within this severely affected group. The current study examined an international sample of 2138 study participants with ME/CFS, of whom 549 were severely affected (operationalized as ‘Homebound’). A subsample of 89 very severely affected participants (operationalized as ‘Homebound-bedridden’) was also examined. The findings showed a significant association between severely and very severely affected participants within the post-exertional malaise (PEM) symptom domain. The implications of these findings are discussed.
________________________________________________________________________________
In-Depth Analysis of the Plasma Proteome in ME/CFS Exposes Disrupted Ephrin-Eph and Immune System Signaling
Arnaud Germain Susan M. Levine and Maureen R. Hanson *
Department of Molecular Biology and Genetics, Cornell University, Ithaca, NY 14853, USA
Proteomes 2021, 9(1), 6; https://doi.org/10.3390/proteomes9010006
Received: 1 January 2021 / Revised: 24 January 2021 / Accepted: 25 January 2021 / Published: 29 January 2021
(This article belongs to the Special Issue Functional Proteomics 2020)
Abstract
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a disabling disease with worldwide prevalence and limited therapies exclusively aimed at treating symptoms. To gain insights into the molecular disruptions in ME/CFS, we utilized an aptamer-based technology that quantified 4790 unique human proteins, allowing us to obtain the largest proteomics dataset yet available for this disease, detecting highly abundant proteins as well as rare proteins over a nine-log dynamic range. We report a pilot study of 20 ME/CFS patients and 20 controls, all females. Significant differences in the levels of 19 proteins between cohorts implicate pathways related to the extracellular matrix, the immune system and cell–cell communication. Outputs of pathway and cluster analyses robustly highlight the ephrin pathway, which is involved in cell–cell signaling and regulation of an expansive variety of biological processes, including axon guidance, angiogenesis, epithelial cell migration, and immune response. Receiver Operating Characteristic (ROC) curve analyses distinguish the plasma proteomes of ME/CFS patients from controls with a high degree of accuracy (Area Under the Curve (AUC) > 0.85), and even higher when using protein ratios (AUC up to 0.95), that include some protein pairs with established biological relevance. Our results illustrate the promise of plasma proteomics for diagnosing and deciphering the molecular basis of ME/CFS.
Brain and Behavior
________________________________________________________________________________
ORIGINAL RESEARCH
Open-label study with the monoamine stabilizer (-)-OSU6162 in myalgic encephalomyelitis/chronic fatigue syndrome
Sara Haghighi, Sara Forsmark, Olof Zachrisson, Arvid Carlsson, Marie K. L. Nilsson, Maria L. Carlsson, Robert C. Schuit, Carl-Gerhard Gottfries
First published: 02 February 2021 https://doi.org/10.1002/brb3.2040
Abstract
Objectives
The purpose of the present study was to investigate the safety and tolerability of the monoaminergic stabilizer (-)-OSU6162 in patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). In addition, a potential therapeutic effect of (-)-OSU6162 in ME/CFS was evaluated by means of observer-rated scales and self-assessment rating scales.
Materials and Methods
In the current study using an open-label single-arm design ME/CFS patient received treatment with (-)-OSU6162 during 12 weeks. The patients received the following doses of (-)-OSU6162: 15 mg b.i.d. during the first 4-week period, up to 30 mg b.i.d. during the second 4-week period and up to 45 mg b.i.d. during the third 4-week period, with follow-up visits after 16 and 20 weeks.
Results
Out of 33 included patients, 28 completed the 12 weeks treatment period. (-)-OSU6162 was well tolerated; only one patient discontinued due to an adverse event. Vital signs and physical examinations showed no abnormal changes. Blood analyses showed an increase in serum prolactin. Therapeutically, improvements were seen on the Clinical Global Impression of Change scale, the FibroFatigue scale, the Mental Fatigue Scale, the Fatigue Severity Scale, Beck Depression Inventory, and the Short Form 36 Health Survey Questionnaire.
Conclusions
(-)-OSU6162 is well tolerated in ME/CFS patients and shows promise as a novel treatment to mitigate fatigue and improve mood and health-related quality of life in ME/CFS. Obviously, the present results need to be confirmed in future placebo-controlled double-blind trials.
________________________________________________________________________________
UK Moves to Revise Guidelines for Treatment of Chronic Fatigue Syndrome
AJN, American Journal of Nursing: March 2021 - Volume 121 - Issue 3 - p 16
doi: 10.1097/01.NAJ.0000737248.67484.2e
Abstract
Advocates hail rejection of debunked exercise and cognitive behavior therapies.
Proposed guidelines for management of myalgic encephalomyelitis, or chronic fatigue syndrome (ME/CFS), from the United Kingdom's National Institute for Health and Care Excellence (NICE) are being hailed for their rejection of graded exercise therapy and cognitive behavior therapy (CBT) as routine treatment. Major medical organizations, advocacy groups, and patients have strongly advocated for NICE to align guidelines with scientific evidence.
The U.S. Centers for Disease Control and Prevention (CDC) in 2017 eliminated these largely useless and, in some cases, harmful therapies from its recommendations. That NICE is now following suit is good news, though many say it is long overdue. Moreover, patients are unlikely to see immediate results as new science can take years to reach clinical practice.
The illness is characterized by debilitating fatigue and difficulty with concentration and memory. An estimated 2.5 million Americans are diagnosed with ME/CFS, most of them women. Because symptoms can range widely and standard laboratory tests yield little insight as to cause, ME/CFS has been viewed as a stress-induced disorder in some women.
Graded exercise therapy and CBT became the go-to therapies for ME/CFS based on findings of a 2011 study, known as PACE, published in the Lancet. According to the study investigators, these treatments produced a sustained improvement in patients' levels of fatigue and physical function, even leading to recovery for some. Top researchers who reviewed the study, however, found major flaws. Patients also reacted negatively, saying the study's results did not reflect their experiences and reinforced inaccurate and stigmatizing beliefs about the illness as a psychological and behavioral disorder. Eventually, over 100 academics, patient groups, and others called for an independent reanalysis of the data. Despite this forceful opposition, the study remained influential with clinicians and continued to underpin treatment recommendations of major medical organizations, including the CDC and NICE.
Perceptions began to change with the 2015 release of the Institute of Medicine's landmark report, Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness, in which the authors described ME/CFS as a “serious, chronic, complex, systemic disease” and cited newly identified biomarkers indicating immunological and neurological dysfunction. The report and continuing pressure from scientists, clinicians, and patients led the CDC to remove recommendations for graded exercise therapy and CBT as its British counterpart, NICE, now proposes to do.--Karen Roush, PhD, RN, FNP-BC, news director

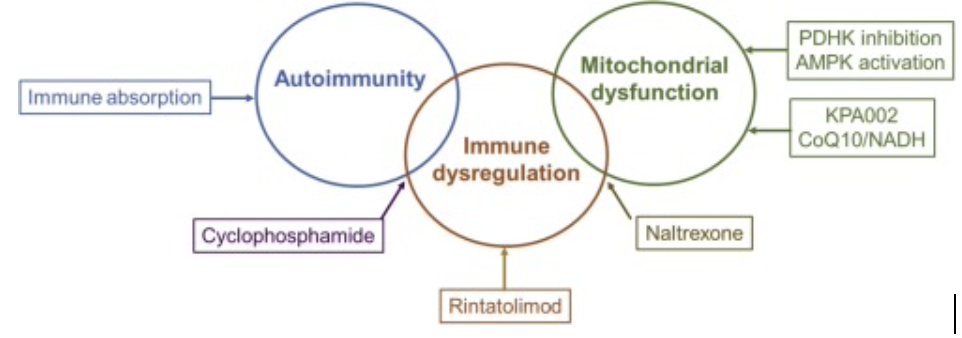
 RSS Feed
RSS Feed